Dental Implants
What happens when a tooth is lost and how can an implant help?
When a tooth is lost, the bone that used to hold the tooth in position begins to dissolve due to lack of stimulation. This causes a decrease in thickness and height of the bone in the area the tooth was lost. Neighboring teeth and opposing teeth may begin to move into the space over time. This causes food trapping, subsequent decay, gum disease and abnormal biting forces being placed on the teeth which could lead to fracture of the tooth which then may need a root canal treatment or extraction. Loss of teeth can also cause the cheek and lips to collapse giving an aged look.
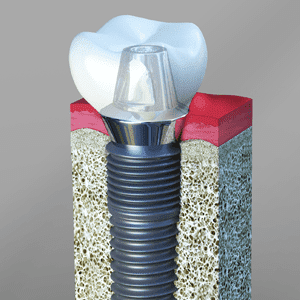
The consequences of tooth loss can be prevented by replacing the lost tooth in a timely manner. Although there are several options to replace a missing tooth, the number one choice for replacing missing teeth is dental implants. A dental implant is a screw made from a titanium alloy that is surgically implanted by the Periodontist into the jaw bone, to replace missing teeth or help secure a denture. Once integrated into the bone, they act like tooth roots onto which small posts (abutments) are attached to, which protrude through the gums. These posts provide stable anchors that your general dentist or prosthodontist can attach a crown, bridge or denture to. Implants can maintain the bone long term by stimulating the bone when you bite on them, and prevents unnecessary trimming of adjoining teeth for bridge placement which could lead to future nerve or decay problems.
Are there Alternative Tooth Replacement options?
Depending on the number of missing teeth, the other tooth replacement options include a Bridge, which utilizes the teeth either side of the space to anchor a permanent fixed false tooth in the space; or a removable denture which utilizes metal clips on other teeth in the mouth or suction to support removable false teeth.
Bridge
Many people who are missing a single tooth opt for a fixed bridge; however, a bridge may require the cutting down of healthy teeth. As the teeth in the bridge are connected together, cleaning in-between the teeth can be trickier, and if you are not careful, decay, nerve and gum problems may arise in the future. This could mean replacement of the bridge down the track, with more additional costs, and could affect the health of the anchoring teeth.
Removable Denture

Another option to replace missing teeth is a removable partial denture or complete denture depending on the number of teeth missing. This is a removable option, where the false teeth are removed each night to allow the gums and teeth to settle down. Metal clips or suction is used to keep the teeth is place. The chewing efficiency with a denture can be reduced, and the teeth that support the partial denture may be weakened in the long term, due to the excessive loads acting on them and eventually could be lost. The denture in some cases also rests on the gum, and may have the potential to cause tissue abrasion and bone loss, particularly if the denture is not fitting correctly. Removable dentures may slip or cause embarrassing clicking sounds while eating or speaking. Studies show that within five to seven years there is a failure rate of up to 30% in teeth located next to a fixed bridge or removable partial denture.
Are there any Long-term Implant Problems?
Since implants are made of titanium, they do not suffer from decay. Implants can however suffer from gum disease or Peri-implantitis, which causes the bone around an implant to dissolve away. This could ultimately lead to loss of the implant and crown. Smokers and people who have had periodontal disease have a 4 times higher risk of developing peri-implantitis. You should discuss your risk with your Periodontist and strategies to help reduce this risk.
Unlike Periodontal disease, treatment of Peri-implantitis is not currently predictable and in some cases, implants may need to be removed. Because of this, it is important that we try and prevent this from happening. Implants can service you for several years or more, and with regular assessment, professional cleaning and proper home care the risk of problems can be reduced.
Who is a candidate for Implants?
Anyone who is missing one or several teeth is a candidate for implants. With the exception of growing children/young adults (less than 20 yrs of age), dental implants are the solution of choice, even with the following conditions:
Existing Medical Conditions:
If you can have routine dental treatment, you can generally have an implant placed. While precautions are advisable for certain conditions, patients with chronic diseases like high blood pressure and diabetes can be candidates for dental implant treatment.
Gum Disease or Problem Teeth:
Almost all implants placed in patients who have lost their teeth to periodontal disease or decay have been successful. If you have had periodontal disease in the past you will however be at higher risk of developing Peri-implantitis and as such is it important to have regular periodontal maintenance cleanings and assessment to reduce the risk of this occurring.
Currently Wearing Partials or Dentures:
Implants can replace removable bridges or dentures, or they can be used to stabilize and secure the denture, making it much more comfortable.
Smokers:
Although smoking lowers the success rate of implants and bone grafting, and increases the risk of Peri-implantitis, it doesn’t eliminate the possibility of having implant treatment. Ideally, you would work to reduce your smoking and ultimately quit, to reduce the risk of possible short-term and long-term complications.
Bone Loss:
Bone loss is not uncommon for people who have lost teeth or had periodontal disease. Periodontists are trained and experienced in grafting bone to safely and permanently secure the implant.
Age:
Tooth replacement with implants in children and young adults is usually deferred until their jaw growth is complete (usually this is in the mid to early twenties depending if you are male or female). There are, however, some instances when a dental implant may be appropriate at a younger age, such as when it is part of the child’s orthodontic treatment plan. Your family dentist or orthodontist can guide you in this instance.
Procedure
An initial assessment of the health of your mouth and teeth is needed prior to implant treatment. If your tooth has not yet been removed, this will need to be done first. When a tooth is removed, the bone in the area shrinks during the healing process. This could produce a situation where there is not enough bone for an implant or extensive bone grafting may be needed. Because of this, it is recommended in a lot of cases to place a bone graft in the tooth socket at the time the tooth is removed. This provides a scaffold for new bone to grow in, while also reducing the amount of bone shrinkage in the area, limiting the potential need for a bigger bone graft later. This bone graft will then need to heal for at least 3 months. A temporary tooth may be made by your general dentist to wear during this healing period.
After the are has healed, usually a Cone Beam CT (CBCT) scan is taken to allow your Periodontist to assess the thickness and height of the jaw bone where the implant will be placed. This also allows the Periodontist to assess where any nerves, blood vessels, sinuses are, and to make sure there is no pathology or abnormalities present.
This initial assessment then allows the Periodontist to select the most appropriate size and shape of an implant, along with assessing if any bone grafting or gum grafting is needed to promote long term implant success.
Dental Implant placement usually takes one or two surgical appointments. The number of appointments may increase if extensive grafting is needed.
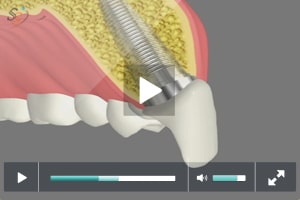
- During the first surgical appointment, the area is ‘numbed up’ and the gum in the area is lifted away from the bone. The implant site is then prepared using drills to create a space (the osteotomy) to receive the implant. This is done following strict aseptic procedures. The implant is then screwed into the prepared site. If the bone around the implant is very firm and solid, a healing abutment may be placed that allows the gum to heal around the implant. If this is the case a small polished cap will be seen at the gum level. If the bone is soft or grafting is done in the same appointment, a cover screw will be placed on top of the implant and the gum tissue is sutured back over the top of the implant. If this is needed, a second surgical procedure (see number 2) will be needed to expose the implant. The implant then requires 4- 6 months to fuse with the bone. If a healing abutment is used, the periodontist will reassess the implant after this time frame and then refer you to your general dentist for the final crown. During the healing time, your general dentist may make you a temporary tooth to wear if needed.
- During the second surgical appointment (4-6 months after implant placement), the implant area is numbed up again and the implant is uncovered. An appropriate healing abutment is attached to the implant and the gums are sutured back in place. After another month or so of healing, the implant is checked and you will be referred back to your general dentist.
Once you are cleared for the final restoration, your general dentist or prosthodontist will take an impression of the implant, and it will be sent to the lab for the fabrication of the implant crown. During this time a temporary crown may be placed. Once the final crown is back, it is cemented with permanent cement or screwed into place. An x-ray is then normally taken after your final crown is placed to ensure the crown is completely seated, assess the bone around the implant and to allow tracking of the health of the implant.
Bone grafting
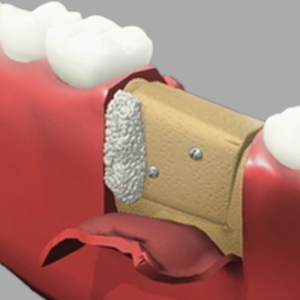
If you have lost bone in the area of the planned implant, we may need to regrow the bone in order to allow an implant to be ideally placed. Depending on the results of a CBCT scan and the amount of bone grafting needed, this bone graft may be done at the same time as implant placement or in a separate procedure. Typically, this will increase the healing time frame up and could add on an additional 6-9 months for the bone to heal if a large graft is required.
During the bone grafting procedure, local anesthetic is placed, the gum is lifted to expose the bone defect. Bone graft particles are then placed in the area the bone is to be grown and covered with a special membrane. The membrane is then fixed into place with small tacks or screws. Typically, donated human bone from a tissue bank is used, however other options such as cow bone or synthetic bone grafting materials may be used instead of or in combination. Once the graft and membrane is placed, the gum released and is then stitched back over and allowed to heal. Releasing the gum to allow space for the bone graft typically causes some bruising and swelling and it is important that you follow your post-operative instructions to reduce this.
Over a period of up to 6-9 months, your bone cells will grow into the area and turn the bone graft particles into your own natural bone. If implants were not able to be placed at the same time as the bone graft, the implants will need to be placed in an additional surgical procedure once the bone has healed.
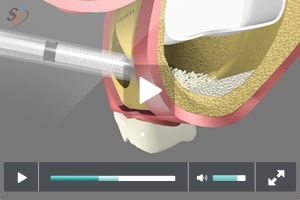
Sinus grafting
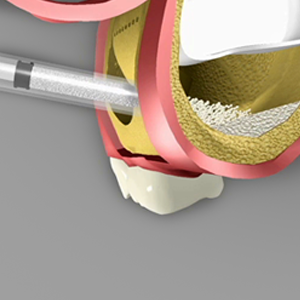
If your teeth have been missing for some time in the top jaw, or bone was lost due to periodontal disease or extraction, there may not be enough bone below the sinus to allow an implant to be placed. In this case the sinus may need to be elevated or pushed up and new bone grown to allow implant placement. Depending on the amount of bone height needed, this may be done at the same time as implant placement or in an additional procedure.
Related Videos