Periodontal Disease
What is periodontal disease?
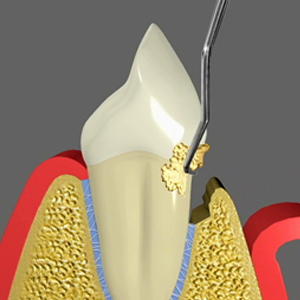
To better understand periodontal diseases and treatment, you first need to understand how a tooth is held in place. The tooth root is attached to the jaw bone by the periodontal ligament. The gum covers the jaw bone and attaches to the periodontal ligament, and forms a collar or cuff around the tooth. Between the gum and the tooth is a naturally occurring pocket or crevice, which encircles the whole tooth. In healthy situations, the depth of this pocket measures 1-3mm and there is no bleeding.
Periodontal diseases (also known as gum disease or periodontitis) can affect one tooth or many teeth, and up to 47% of the population have some form of gum disease. It is a chronic (long-term) infection in the gums which, over a period of time causes the bone, gum and ligament that holds the tooth in place to dissolve away.
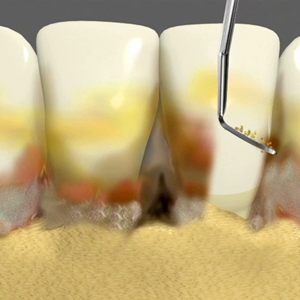
Periodontal disease is primarily caused by bacteria that live in the mouth. Bacteria start to stick together and form what is called plaque. Over time, and with less than ideal oral hygiene (brushing, flossing etc), more and more bacteria begin to grow in the mouth, and the plaque spreads to cover the tooth surface above and below the gums. The bacteria then release toxins into the surrounding gum, ligament and bone. When this plaque mixes with your saliva and food, it can turn into a hard substance called calculus, tartar or scale, which can promote even more bacteria to grow. The bacteria and their toxins cause the gums to swell, appear puffy and bleed easily. This early stage of gum inflammation is called gingivitis. There is usually little or no discomfort. Gingivitis is often caused by poor oral hygiene. Gingivitis is reversible with regular professional treatment and good oral home care.
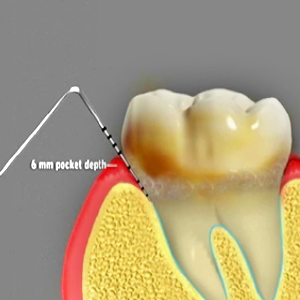
If the inflammation and infection in the gums happens over a longer period of time, Gingivitis may turn into Periodontitis (Periodontal disease), where the infection now involves the gum, bone and the periodontal ligament. The gums separate from teeth, forming periodontal pockets (spaces between the teeth and gums) that become infected. As the disease progresses, the pockets become deeper and more gum tissue and bone are dissolved and destroyed. Symptoms may include bleeding, bad taste in the mouth, bad breath, pain and sensitivity, gum abscesses, tooth mobility, and gum recession. It is not uncommon that people may have no symptoms at all until their gum disease is very advanced, and as such, Periodontal disease can be a ‘silent killer’ of teeth. As a consequence, the gum can recede or shrink around the tooth, exposing the root surface, and the tooth begins to become wobbly, and ultimately the tooth can fall out.
Some individuals are more susceptible to periodontitis due to their genetics. Their genes may affect the ways in which their body attacks this infection, and so rather than just killing the bacteria, the gum and bone around a tooth is also dissolved. Diabetes and Smoking can also make you more susceptible to periodontitis by also affecting the way your body deals with infections. Smoking alone can increase your risk of having periodontal disease by 4 times than if you did not smoke. The infection in your gums can also travel into your blood, and has been shown to have effects on heart disease, stroke, respiratory (breathing) diseases, pregnancy and diabetes. Because of these whole body effects, it is important that periodontal disease is assessed and addressed.
How do you treat periodontal disease?
Assessment:
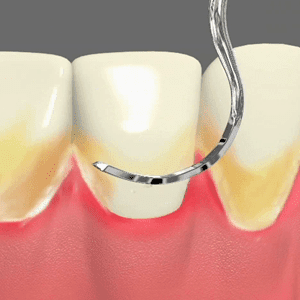
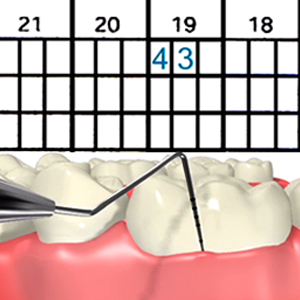
The first stage in periodontal disease treatment is assessment of your gum health. A Periodontist, Dentist or Hygienist assesses the health of your gums by measuring or probing around your teeth. The purpose of this is to record the pocket depth around your tooth, or where your gum attaches to the tooth root. This will allow us to see if it is in a normal position or not.
Normally, a crevice or gutter is present around the tooth, with the gum attaching to the tooth root normally occurring 1-3mm from the tip of the gum. If this measurement is greater than 3mm, a periodontal pocket may be present which can indicate the presence of Periodontal disease. The dentist will also assess how well you clean your teeth at home (amount of plaque present), if you have any early disease signs such as bleeding from the gums, how firm your teeth are in your jaw, and how your teeth bite together. If there are any abnormal findings, these will be discussed and explained to you, along with recommendations for any treatment.
Non-surgical treatment:
Treatment usually begins with non-surgical treatment. This can be done with your Periodontist, general dentist or dental hygienist. However, if your gum disease is severe or advanced, treatment by a specialist periodontist is recommended.
Non-surgical treatment is also called scaling and root planing or deep cleaning. The aim is to clean the teeth above and below the gums to remove the bacteria and the calculus that is causing the gum infection. The gum is ‘numbed up’ using local anesthetic so you will not feel any pain or sensitivity during the procedure. Then the teeth and roots are meticulously cleaned using similar instruments that you would have experienced in the past when having a standard clean (hand instruments and ultrasonic cleaners). The difference however between standard cleaning and Scaling and root Planing, is that the cleaning extends deep under the gum line to where the root attaches to the gum and bone. This does not happen in a standard clean which usually stays above the gums only. In rare occasions, antibiotics and mouth washes may be prescribed to help with disinfecting your mouth and aid in gum healing.
The majority of patients with periodontal disease do not have an ideal home cleaning routine (brushing and flossing) which has allowed the periodontal disease to develop over time. Improving and becoming very focused on your home oral hygiene is very essential to ensure that the gums heal appropriately and help reduce the possibility that the periodontal disease will return in the future. The dental team will assess how good your oral hygiene is and give you recommendations and tools to help improve it. Most people are not effective at cleaning in-between their teeth, which is where the periodontal disease usually starts. An interdental brush most likely will be recommended to you, and is a little pipe cleaner-like brush that fits between your teeth. It is a fantastic tool to help keep the ‘in-between’ areas of your teeth clean, where your tooth brush cannot reach.
After the deep cleaning has been completed, the gums are allowed to heal for 1 to 2 months and then the gums are remeasured to see if the periodontal pockets have shrunk back to normal. If you have gingivitis, then most likely this is all the active treatment you will need. If you have periodontal disease and there are still some bleeding areas and deep pockets above 5mm, gum surgery may be needed to remove the infection, promote stable gum health for the future and give you better access for your cleaning at home.
Surgical Treatment:
A deep pocket above 5mm can increase the risk of having further periodontal disease in the future. It may be necessary to do gum surgery to reduce these pockets and adequately remove the infection. Here the gums are ‘numbed up’with local anesthetic, and are lifted away from the tooth so that the whole tooth root can be seen. Plaque and calculus are then cleaned from the roots in a similar manner as in non-surgical cleaning. At times, the bone around the tooth may not be smooth, with rough and jagged areas being present which can prevent the gum from being ideally positioned around the tooth. In these situations, the bone is smoothed with a drill, so that the gum can then be repositioned tight around the tooth and the periodontal pocket reduced.
Sometimes a bone crater exists around the tooth. In some cases, new bone and gum attachment may be regrown through the use of a periodontal regeneration. A combination of natural or synthetic bone is placed in the crater to fill the space and promote bone growth. Sometimes specialized membranes may be used to cover the bone graft, preventing the gum tissue from creeping in between the tooth and the bone and disrupting the healing. This helps allow regeneration or regrowth of new bone and periodontal ligament. If this is possible, your periodontist will speak to you about this.
Following this, the gums are stitched back lower down and tightly around the tooth, and allowed to heal. After 2-6 months, the gums will be remeasured to assess the healing. Most people will experience some gum recession, and the spaces between their teeth will be bigger. This is normal, and allows easier access for cleaning, along with reducing the periodontal pocket to a normal maintainable range. Some temperature sensitivity is to be expected following gum surgery, and usually subsides over the coming months. A sensitive tooth paste can help with this until it settles.
Periodontal Maintenance:
Once the periodontist is happy with the health of the gums, the Periodontist and Dental Hygienist will work together with your general dentist to maintain your oral health and reduce the risk that the Periodontal disease will come back. This is done through regular periodontal maintenance, and is a very important part of ensuring the disease does not return. Initially, the Periodontist and Dental hygienist will see you generally every 3-4 months to check how well your home cleaning is going, offer tips and support to improve it, reassess your gum measurements, and remove any plaque and calculus that you were unable to clean off at home. This is to prevent the bacteria growing back under your gums and allowing the infection to start again.
If your home cleaning is going well and your gums are remaining healthy, your Periodontist may decide to alternate maintenance cleanings between our office and your general dentist. The frequency of this will depend on each patient and how well your home cleaning and gums are doing. Periodontal maintenance will need to be done frequently for the rest of your life, as unfortunately periodontal disease can come back if bacteria are allowed to grow again.




